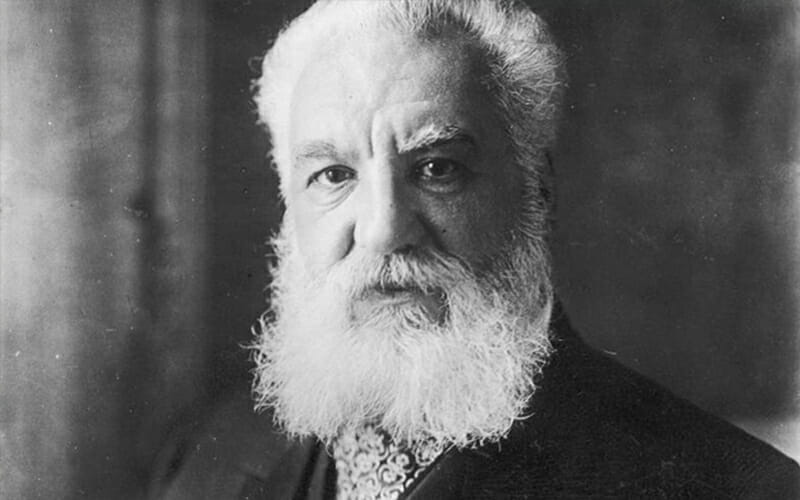
Sir Frederick Grant Banting
Sir Frederick Grant Banting, physician, surgeon, army officer, medical researcher, Nobel laureate, and artist; b. 14 Nov. 1891 in Essa Township, Simcoe County, Ont., son of William Thompson Banting and Margaret Grant; m. first 4 June 1924 Marion Wilson Robertson in Toronto, and they had a son; they divorced 2 Dec. 1932; m. secondly there 2 June 1939 Henrietta Elizabeth Ball; they had no children; d. 21 Feb. 1941 near Musgrave Harbour, Nfld.
Fred Banting was a child of agricultural Ontario, the youngest of six born on the family farm near Alliston, northwest of Toronto. A shy, quiet boy who liked athletics and animals, he was encouraged by his family to continue his education beyond the local schools. In 1910 he enrolled in general arts at Victoria College in the University of Toronto, was not able to pass all his subjects, and while repeating the year, dropped out after learning he could enter the faculty of medicine. Medicine had vied with the Methodist ministry as a possible profession.
Banting began his medical course in 1912. He received slightly higher-than-average grades but otherwise did not stand out. The five-year program in medicine was radically condensed during World War I. He graduated with a bachelor’s degree in December 1916. By his own account, Banting had not been particularly well trained. He had developed an interest in surgery, enlisted in the Canadian Army Medical Corps, and upon graduation began full-time military service. He worked as a surgeon in a Canadian hospital in England for 13 months, was sent to France in June 1918, and as a battalion medical officer, served on the front lines during fierce fighting that summer and autumn. In the attack on Cambrai on 28 September Captain Banting was hit in his right arm by shrapnel and evacuated. He was awarded the Military Cross for his conduct during the action. After several weeks of anxiety about the condition of his wound, Banting was able to resume duties in England, before being recalled to Canada in 1919.
He had shown interest in improving his medical qualifications and dabbling in research. In 1919-20 he worked under one of his wartime mentors, Clarence Leslie Starr, as a senior house surgeon and registrar at Toronto’s Hospital for Sick Children. He hoped to specialize in orthopedic surgery. When his appointment was not renewed – the reason is not clear – Banting decided to practise medicine as a general physician and surgeon. In July 1920 he hung out his shingle in the prosperous small city of London, west of Toronto, and waited for patients to come.
When they were discouragingly slow in doing so, Banting took on part-time work as a demonstrator in surgery and anatomy in the small faculty of medicine at the University of Western Ontario. He was deeply worried about his financial affairs, his practice, and his marital prospects, and began wondering if there were better courses to follow. As he prepared to give a talk to Western students about the pancreas, Banting happened, on the night of 31 Oct. 1920, upon an article in the November issue of the journal Surgery, Gynecology and Obstetrics (Chicago) by pathologist Moses Barron entitled “The relation of the islets of Langerhans to diabetes with special reference to cases of pancreatic lithiasis.” Some of Barron’s observations about an unusual but unimportant case of blockage of the pancreatic duct inspired Banting to reflect upon scientists’ search for a substance in the pancreas that might hold the key to preventing the disease known as diabetes mellitus. Late that night he jotted in his notebook a research idea:
- Diabetes
- Ligate pancreatic ducts of dog. Keep dogs alive till acini degenerate leaving Islets. Try to isolate the internal secretion of these to relieve glycosuria
Staff at Western, who lacked both expertise and facilities, advised Banting to discuss his idea with the professor of physiology at the University of Toronto, John James Rickard Macleod*, an internationally recognized expert in carbohydrate metabolism. At a meeting in Toronto on 8 November, Macleod told Banting, who had little knowledge of either diabetes or the pancreas, that his idea could be worth pursuing, but might well lead to the same negative results that had bedevilled many more-experienced researchers. If Banting still wanted to try, Macleod would make facilities and animals available to him.
Banting blew hot and cold about the research idea that winter. He later wrote that his preference would have been to take a job as a medical officer on an expedition searching for oil in the Canadian north. Friends advised him to settle down and make the best of a practice that was growing decently. Instead, he decided to take advantage of Macleod’s offer and spend the summer of 1921 working in Toronto on his idea. Macleod gave him laboratory space, a supply of research animals, and the services of his student assistants. Charles Herbert Best* won a coin toss with Edward Clark Noble to be the first to work with Banting, and both later agreed that Best would stay on for the summer. Banting and Best began work on 17 May.
Banting believed that by ligating the pancreatic ducts of living animals, he could cause the cells that produced the organ’s external secretion (digestive enzymes) to degenerate. They would no longer interfere with or neutralize the pancreas’s mysterious internal secretion, which could then perhaps be isolated in an active form. Evidence from his notebook and later suggests that Banting first hoped to use his surgical skills to transplant portions of the pancreas from duct-ligated dogs to diabetic dogs to see if he could improve their condition by reducing the sugar in their urine or blood. The research proceeded slowly and fitfully through the hot summer of 1921, with heavy loss of animals and various setbacks, frustrations, and transient frictions between Banting and his assistant. After the first month, during which he gave advice and instructions to Banting, Macleod had gone to Scotland for the rest of the summer.
By the end of July, Banting and Best, in lieu of transplants, were able to begin injecting extracts from the pancreas of duct-ligated dogs into the veins of depancreatized, diabetic dogs. The dogs’ blood sugars appeared to drop dramatically, suggesting that the extracts were restoring the metabolic function. In some cases, the animals were perkier and lived a little longer than would normally be expected with untreated diabetes. When he returned from Scotland in September, Macleod urged an enthusiastic Banting to build his evidence by repeating and refining his experiments. Unfortunately, Banting and Macleod, the one untrained and bluntly impulsive personality, the other a cautious and quiet scientist, disagreed sharply about the priority that Banting’s work should have. A serious breach was narrowly avoided, and the work continued through the autumn.
Banting found that he could bypass his cumbersome duct-ligation procedure by making extracts from fresh fetal calf pancreas. Then he found that chilled extracts of whole dog or beef pancreas could also be effective. As the pace of the research increased – from the beginning Banting’s goal was to be able to treat “diabetus” in humans – he suggested that the team be strengthened by the addition of James Bertram Collip*, an experienced biochemist who was working with Macleod in Toronto while on leave from the University of Alberta. Collip joined the group in December, quickly began making improvements in Banting and Best’s crude extract, and added substantially to knowledge of its properties. Still, the first formal presentation of the Toronto group’s findings, at the annual conference of the American Physiological Society in New Haven, Conn., on 30 December, was far from triumphant, as there was considerable doubt that the team had gone further with pancreatic extracts than several previous investigators.
Even as the research then advanced to another level, it was hampered by Banting’s deep insecurity and mounting suspicion that Macleod and perhaps others were appropriating credit for his findings. He resented the extent to which Macleod publicly identified himself with the work and became deeply alarmed when Collip was given the responsibility of purifying the extract for use in clinical trials. Macleod granted Banting’s demand that his and Best’s extract be the one first used formally on a human diabetic (Banting earlier had tried it on himself and a diabetic classmate with meaningless results). The initial test was made on 11 Jan. 1922 on a 13-year-old boy, Leonard Thompson, in the Toronto General Hospital. Banting was not present; lacking experience with diabetes, he had been denied privileges at the university’s teaching hospital.
Banting and Best’s extract had only minor effects on Thompson’s condition, and a sterile abscess formed at the site of injection. The clinicians decided to discontinue the experiment. Twelve days later, on 23 January, they resumed administration, but with an extract that had been purified by Collip. When Collip told Banting of the favourable results of his extract and then refused to reveal details about his method of making it, the two scientists came to blows in the lab and Best had to separate them.
On 25 January the four researchers signed an agreement to work together, under Macleod’s general direction and in cooperation with the University of Toronto’s Connaught Antitoxin Laboratories [see John Gerald FitzGerald*], to develop the extract. Collip would be in charge of production. It was separately agreed that the names on publications would be in alphabetical order.
Harmony was never fully restored to the research team, even as the first clinical trials began to yield truly exciting results. The purified extract, soon to be named insulin after the cells in the pancreas known as the islets of Langerhans, where the group assumed it originated, had dramatic effects in eliminating the symptoms of diabetes mellitus and restoring its victims to nearly normal physical health. A very great discovery was emerging from the University of Toronto. Who had made it?
Banting believed that he was the discoverer of insulin, first as the man whose idea led to the discovery, and secondly as the conductor of the animal experiments which he believed had proved the presence of the substance. His claim was highly vulnerable, however, because of inadequate controls and inconsistent results in his research, the failure of his extract in the first Thompson trial, and the inconclusive result of a longevity experiment on one of the dogs (whose pancreas Banting had failed to remove completely). At the time there was a prima facie case that Collip’s work had made the great leap forward in Toronto. Later analysis has supported this view, exposing numerous factual and interpretive errors in Banting and Best’s first paper, Banting’s mistaken assumptions about the physiological consequences of duct ligation and pancreatic degeneration, and the possibility that faulty technique made their experiments almost meaningless. As well, Macleod had given Banting more advice than the latter acknowledged. As early as December 1922 the British Medical Journal (London) published a devastating critique of Banting and Best’s research, which concluded that “the production of insulin originated in a wrongly conceived, wrongly conducted, and wrongly interpreted series of experiments.”
Banting, who had risked his career, his livelihood, his reputation, and perhaps the possibility of marital happiness on the research, had nearly broken down in the early months of 1922. He seldom appeared in the lab and, by his own account, used alcohol, sometimes stolen from the lab, to get to sleep. Friends thought he might be suicidal. He returned to work, however, at Best’s urging after Collip found that he had lost the ability to produce effective insulin, a not-uncommon problem in pioneering biochemical extraction. A desperate struggle by the team in the spring to rediscover the technique resulted in Banting and Best recovering an element of leadership: Banting suddenly found himself with the major supply of usable insulin – made by Best – and both his morale and his determination revived. He felt deeply indebted to Best for having come to his aid when he most needed it, and he launched into private practice in Toronto as the clinician who could treat diabetes and was also permitted to care for diabetic patients at the Christie Street military hospital.
A tense, confusing situation was gradually resolved as Banting received an appointment at the Toronto General Hospital to work with other clinicians on its diabetes ward. The process of isolating insulin was patented in the names of Banting, Best, and Collip and the patent then transferred to the University of Toronto’s board of governors. A joint venture between the university and Eli Lilly and Company of Indiana resulted by the summer of 1922 in a constantly growing supply of effective insulin, which began to be used in informal clinical trials in several centres. Collip returned to the University of Alberta. Macleod concentrated on researching the physiological properties of insulin. The Connaught Laboratories gradually assumed control of Canadian insulin production.
By the end of 1922, it was clear that insulin’s impact on the treatment of diabetes was dazzling, and the discovery was almost universally hailed as a triumph of modern medicine. With important help from politically astute friends and admirers such as his former teacher Dr George William Ross, Banting quickly developed a reputation as the key man in the insulin story, a rough-hewn Canadian genius who had taken his idea to wonderful success under the most difficult conditions, with some assistance from Best. An organized campaign to honour Banting led to the government of Ontario in 1923 appointing him as a Banting and Best chair of medical research at the University of Toronto, the first purely research professorship at a Canadian university. Parliament granted him an annuity “sufficient to permit Dr. Banting to devote his life to medical research.” In the autumn of 1923, it was announced that Banting and J. J. R. Macleod would share that year’s Nobel Prize in Physiology or Medicine for the discovery of insulin. It was the fastest honouring of discovery in the history of the Nobel prizes; Banting, at the age of 31, was the youngest laureate and the first Canadian. For the rest of his life, he would head lists of prominent Canadians, and he would be showered with honorary degrees, prizes, and fellowships.
He remained embittered at almost everything to do with Macleod’s role in the research, briefly considered rejecting the Nobel, and then declared that he would share his prize money with Best. Macleod said that he would divide his with Collip. For many years there was general curiosity about what had happened in Toronto to cause such a strange and controversial situation – two prize winners, and four equal sharers in the money. At the University of Toronto’s celebratory banquet on 26 November, Dr Llewellys Franklin Barker tactfully summarized the controversy with the comment “There is in insulin glory enough for all.”
The two Nobel laureates went separate ways at the university and were said not to speak. In 1928 Macleod returned to his native Scotland, and Best, who had left Toronto to finish his education in Britain, was appointed to Macleod’s chair in physiology the following year. Banting had resumed research in facilities separate from the department. An adoring public and media wondered what diseases the Canadian genius would next conquer. To help him, his admirers in 1925 raised $500,000 to endow Canada’s first medical research fund, the recently created Banting Research Foundation. Banting at first worked mainly in solitude, assisted by Sadie Gairns, who had done an MA with Macleod. His aura and the funding he could command gradually attracted other researchers, his chair evolved into the Banting and Best Department of Medical Research, and by the 1930s it had become one of the largest university research establishments in North America.
Banting saw himself as an idea-driven man, not a clinician or a diabetes specialist. He deeply wanted to make further discoveries on his own to show that the doubts about his competence in the insulin work were wrong. It was unfortunately true that his training had been inadequate and his later research ideas and techniques were crude, simplistic, and unproductive. A quest to produce a universal antitoxin, initially billed as something better than insulin, from the secretions of the adrenal cortex was a dismal failure. Banting then took up cancer research, devoting years of fruitless experimentation to the problem of Rous sarcoma in chickens. His obsession with ideas that might lead to the catching of another brass ring, somewhat on the model of tinkering inventors, led to investigations of infant stools, royal jelly, the physiology of drowning, and other unproductive initiatives.
Several of the workers around Banting were better trained and began making significant contributions. In the 1930s his department, administered by Gairns and with quarters in a larger building misleadingly named the Banting Institute, was a major pioneer in developing a state-of-the-art preventive approach to silicosis. Banting’s self-effacing position on research – he gradually recognized and accepted his limitations – made him popular with his young associates. As the great discoverer of insulin, he slipped naturally, if a bit awkwardly, into a broader role as national spokesman for medical research. In 1937 he was asked to join the National Research Council, chaired by former army chief of staff Andrew George Latta McNaughton*, and the next year he became head of its new Associate Committee on Medical Research, the first body charged with national responsibility for coordinating work in Canada.
Banting’s tribulations as a researcher were paralleled by a less-than-happy personal life. In the turmoil of the insulin years, a relationship with his Alliston sweetheart had collapsed. The marriage in 1924 of Canada’s most eligible bachelor with an outgoing doctor’s daughter, Marion Robertson, proved an ill-considered joint imprisonment in solitudes, loneliness, and deep unhappiness. It formally ended in 1932 in a sensational divorce, with charges and countercharges of adultery and abuse. Accused publicly by his father-in-law of beating his wife, Banting struck back with private threats to deny the paternity of their son. During these years he found refuge in painting, developing through Toronto’s Arts and Letters Club friendships with Alexander Young Jackson* and several other members of the Group of Seven, whose techniques he competently absorbed. He went on several sketching trips with Jackson, including a lengthy visit to the Arctic in 1927. In the subjects of his art, in his attitudes to women, and in his musings about the stresses of his fame, Banting often expressed nostalgia for the simpler life and mores of rural Canada.
In 1934 he was one of the last group of Canadians who received titles from the monarch. He hoped his knighthood was the exoneration of his tarnished standing as a divorcé, but otherwise thought it ludicrous for people to address him as “Sir.” His friends appreciated him as just one of the gang, an amiable storyteller, especially late in the night while killing a bottle of rye in a smoke-filled room. It was often remarked, sometimes by Banting himself, that he would have been happiest in medicine as a general practitioner in a small town. Still hoping to find contentment in marriage and to father a flock of children, in 1939 he married Henrietta Ball, who had been working as a technician in his department.
He had become well-travelled and a frequent diarist, who recorded strong opinions on the state of the world, the problems of his fame, and the conundrums of life in Canada. In 1935 he attended a physiological congress in the Soviet Union, toured widely, and came home with the enthusiasms of a typical fellow-traveller who thought he had seen the future, at least concerning socialism’s recognition of science. As the world drifted towards another war, Banting tried to alert the British government to the need for serious initiatives to prepare for bacterial and chemical warfare against Adolf Hitler. In 1939 he converted his department’s research focus to problems in aviation medicine, while also re-enlisting in the Canadian Army.
Banting spent several months in Britain during the winter of 1939-40 trying to assess research needs. At home, he threw himself into war work at every level, from useful advances in aviation medicine through quixotic studies of bacterial warfare and self-wounding with mustard gas to test an antidote. As the Battle of Britain developed, he longed to be able to resume the simple role of a medical officer with his old battalion, or at least to get back to England in its time of crisis. His relationship with Charles Best, who had been forging a parallel career at the University of Toronto and in medical research circles, had become cool and testy (in marked contrast to the friendship Banting developed with J. B. Collip). When Best said that he could not go to Britain on the next research liaison mission, Banting decided to go instead. To reduce travel time he took up a casual offer of a ride on a bomber being ferried across the North Atlantic.
He left Gander, Nfld, on a two-engine Hudson with a crew of three during the night of 20 Feb. 1941. Shortly after take-off, the pilot reported that an engine had failed and he was turning back. When the second engine failed, the plane crash-landed by a pond near Musgrave Harbour, on the east coast of Newfoundland. Two of the crew were killed instantly. The pilot survived. Banting was mortally injured and died before outside help arrived.
Major Sir Frederick Banting’s body was returned to Toronto, where he was given a hero’s and a warrior’s funeral. There is no truth in propaganda stories that he had been on a secret mission to Britain of the highest importance, or in persistent rumours that his plane had somehow been sabotaged by Nazi agents. He left a modest estate to his widow and the son of his first marriage.
Over the years Banting’s fame remained undiminished, as the myth persisted that insulin had been discovered through the genius of Banting and Best, working without significant help. He had been the curious and lucky doctor who had started a ball rolling, had stayed with it through the mobilization of expert help in an excellent facility, and then had spent the rest of his life coping with the consequences of having achieved a scientist’s fondest dream – saving lives, winning the Nobel Prize, becoming an immortal.
The Sir Frederick Grant Banting papers (ms coll. 76) in the Thomas Fisher Rare Book Library, Univ. of Toronto, are the major manuscript source covering all aspects of Banting’s life. They are particularly rich in documentation about the discovery of insulin, including all of his and Best’s laboratory notebooks, patient records, and other research materials, as well as scrapbooks and Banting’s two personal accounts of the discovery, only one of which has been published. They also contain his diaries and other unpublished writings, among which are his extensive war diaries. Sir Frederick Banting’s papers relating to his work at the National Research Council Can. in Ottawa are held in its archives and library.
The Fisher Library holds other important collections related to the discovery of insulin, including the papers of Charles Herbert Best (ms coll. 241) and James Bertram Collip (ms coll. 269), as well as material assembled by William R. Feasby (ms coll. 235) and this author, Michael Bliss (ms coll. 232). The impact of the discovery on one patient’s life is demonstrated in the Elizabeth Hughes papers (ms coll. 334). The most recent addition (2012) to the Fisher collections on insulin is the George William Ross papers, consisting of interviews and manuscripts generated by a close friend of Banting’s who led the campaign to have him honoured and tried to be his first biographer. Univ. of Toronto, Arch. and Records Management Services also holds relevant collections, including the records of the insulin committee of the university’s board of governors (A1980-0027, A1981-0004, A1981-0005, A1981-0015, A1981-0019, A1982-0001). The Toronto material is described and sampled on the website “The discovery and early development of insulin”: link.library.utoronto.ca/insulin (consulted 8 Oct. 2014).
These and other sources form the basis of the standard published history by Michael Bliss, The Discovery of Insulin (Toronto, 1982; 25th anniversary ed., 2007), which contains extensive bibliographical references. The popularization Breakthrough: Banting, Best and the Race to Save Millions of Diabetics (Toronto, 2010), by Thea Cooper and Arthur Ainsberg, is heavily fictionalized.
The first published biographies of Banting were Banting’s Miracle: The Story of the Discoverer of Insulin (Toronto and Vancouver, 1946) by Seale Harris and Sir Frederick Banting (Toronto, 1946) by Lloyd Stevenson. These were superseded by Michael Bliss, Banting: a biography (Toronto, 1984; 2nd ed., 1992), which remains the standard account and contains a bibliography of Banting’s writings. It may be supplemented with “Banting’s, Best’s, and Collip’s accounts of the discovery of insulin,” intro. Michael Bliss, Bull. of the Hist. of Medicine (Baltimore, Md), 56 (1982): 554-68; J. J. R. Macleod’s “History of the researches leading to the discovery of insulin,” intro. L. G. Stevenson, Bull. of the Hist. of Medicine, 52 (1978): 295-312; and Michael Bliss, “Rewriting medical history: Charles Best and the Banting and Best myth,” Journal of the Hist. of Medicine and Allied Sciences (New Haven, Conn.), 48 (1993): 253-74.
Scholarly studies of Banting as a Canadian hero are K. F. Quinn, “Banting and his biographers: maker of miracles, maker of myth,” Queen’s Quarterly (Kingston, Ont.), 89 (1982): 243-59, and Mary Vipond, “A Canadian hero of the 1920s: Dr. Frederick G. Banting,” Canadian Hist. Rev. (Toronto), 63 (1982): 461-86. Banting’s role in the history of chemical-bacterial warfare in Canada is detailed in John Bryden, Deadly Allies: Canada’s Secret War, 1937-1947 (Toronto, 1989).
Arch. of Ont. (Toronto), RG 80-5-0-1428, no.2088.
© 2018-2021 University of Toronto/Université Laval
Charles Best
CC CH CBE FRS FRSC FRCP (February 27, 1899 – March 31, 1978)
Charles Best was born February 27, 1899, the second of 2 children of Herbert and Lulu (Fisher) Best, younger brother of Hilda. His parents were Canadian but lived in West Pembroke, Maine, where Herbert was a country doctor. Charley would often assist him with patient house calls, in charge of the horse and carriage as they travelled both sides of the Maine/New Brunswick border.
Charley came to Toronto in 1915 to continue his studies at Harbord Collegiate Institute. Though they did not know each other at the time, his future wife, Margaret Mahon, was also a student at Harbord. In 1916, Charley began his studies at the University of Toronto. He was inspired to study medicine by his father and by his Aunt Anna, a nurse who died from diabetes.
At the age of 17 during World War I, Charley enlisted in the 70th Battery of the Horse Artillery and was sent to Camp Petawawa on the Ottawa River. In October 1918, he was stationed in North Wales for training; The War ended the next month before he was sent to France. Once back in Canada, Charley continued with his studies in Physiology and Biochemistry at the University of Toronto.
In 1921, Dr. Frederick Banting, a young physician from London, Ontario, was given lab space at the University of Toronto to pursue his ideas regarding the treatment of diabetes. He needed an assistant to carry out the chemistry procedures. Professor J.J.R. Macleod, head of the physiology department, arranged for Charley Best, one of his top students, to work with Banting. On May 17th, the day after Charley completed his degree, Banting and Best began what would become an extraordinary research and working relationship that led to the discovery of insulin.
Neither Banting nor Best received a stipend, so to help support themselves Charley sold his grandfather’s gold pocket watch, and Banting sold his car. There were many sleepless nights, extensive trials with dogs, and testing with extracts. Over the summer and into the fall they produced good and promising results. They were able to isolate and extract an internal secretion of the pancreas, which was effective in decreasing the blood sugar level of diabetic dogs. Henry Mahon, Charley’s soon-to-be brother-in-law, was at hand with his camera to capture the moment when both men and a test dog posed on the roof at the University of Toronto.
In January 1922, Charley and Fred tested their serum on themselves before giving it to a young Leonard Thomson, who became the first diabetic patient to receive insulin. Leonard’s physical health started to improve almost immediately. In 1923, Banting and Macleod were awarded the Nobel Prize in medicine. Banting subsequently sent a telegram to Harvard where Best was giving a talk about the discovery. It read: “I assign to Best equal share discovery Insulin. Hurt that Nobel Trustees did not so acknowledge him. Will share with him. Please read this telegram at any dinner or meeting. Banting.” Years later the Nobel Committee acknowledged that Best should have been officially recognized. Banting did share the Nobel prize money with Best, who used it to buy a house with his new wife, Margaret.
Following the discovery, Best was head of insulin production at the Connaught Laboratories in Toronto, ensuring it became widely available for the treatment of diabetes. To maintain quality control over the production and sale of insulin, a patent was taken out in the names of Banting, Best and James Collip. The patent was sold for $1.00 to the University of Toronto, who in turn would licence production. Best always jokingly said they never received the $1.00. He continued his studies at the Universities of Toronto and later London (England) under the guidance of Sir Henry Dale.
In 1928, he became head of the Department of Physiological Hygiene (Public Health) at the University of Toronto, and in 1929 he became head of the Department of Physiology at age 30, a position he held for 35 years.
In the 1930s Charley and Margaret had two sons, Sandy and Henry.
Charles Best’s entire life was dedicated to medical research, which included several significant research breakthroughs that put him on the front line of scientific achievement, for example: the discovery of the enzyme histaminase in 1929, the discovery of the role of the B vitamin choline in 1932, and the purification of heparin in 1935. For his work on heparin and choline, he was nominated for the Nobel Prize in 1950.
He also helped launch and develop the dried blood serum project in 1939, and Red Cross blood donor clinics as a result. As Surgeon Lieutenant Commander in the Royal Canadian Navy, he researched night vision and sea sickness.
Fred Banting, sadly and tragically died in a plane crash in Newfoundland, while en route to England in 1941. Best then became head of the Banting and Best Department of Medical Research at the University of Toronto, a role he held until his retirement in 1967.
Throughout his life, he became a mentor to hundreds of students passing through the University of Toronto. During two world tours and many lectures and conferences, he and Margaret met many remarkable academics and scientists who they called friends.
In recognition of his work, he was the recipient of many honorary degrees and held several medical consulting roles, including with the United Nations World Health Organization. In 1971, he was presented with the medal of the Companion of Honour by Queen Elizabeth II. He had a private audience with the Queen and said she was very knowledgeable about medicine.
Away from medical research, he enjoyed painting and was influenced by the Group of Seven and Emily Carr. He painted landscapes of Quebec, PEI, Nova Scotia, New Brunswick and Maine. He also enjoyed sports and was part of the Georgetown baseball team with his friend Clark Noble. Golf was a favourite pastime for Charley, especially for the socializing aspect.
When asked by a young student what some of his favourite things were, he replied: “apple pie and spending time with my grandchildren”.
Towards the end of his life, he took up the piano and had regular lessons with his daughter-in-law, Eileen.
Upon hearing the news of the sudden death of his son Sandy, he collapsed, dying a week later on March 31, 1978.
The discovery of insulin changed Banting and Best’s life, as well as everyone involved, including the millions of diabetics who had their lives transformed.
John Macleod
John James Rickard MacLeod, a physiologist, university teacher, author, and Nobel laureate; born September 6, 1876, in Clunie, parish of Caputh, Perthshire, Scotland, eldest child of the Reverend Robert Macleod and Jane Guthrie McWalter; m. 22 July 1903 Mary Watson McWalter, a second cousin, in Paisley, Scotland; they had no children; d. 16 March 1935 in Bieldside (Aberdeen), Scotland.
A son of the manse, J. J. R. Macleod chose science as his profession and North America as his home. He was educated at the Aberdeen Grammar School and in medicine at Marischal College, University of Aberdeen. After graduate studies at Leipzig and Cambridge and a brief appointment at the London Hospital Medical College, he emigrated in 1903 to become a professor of physiology at Western Reserve University in Cleveland, Ohio. Over the next 15 years, he proved himself a prolific researcher, a learned professor, and an accomplished scientific writer at both the advanced and the introductory levels. His research interests came to centre on metabolism, with special emphasis on the body’s use of carbohydrates. His early books included Diabetes: Its Pathological Physiology (London, 1913) and what became a standard textbook, Physiology and Biochemistry in Modern Medicine (St Louis, Mo., 1918).
Partly out of a desire to return to British soil, as Canada was then perceived, Macleod accepted the offer of the chair in physiology at the University of Toronto in 1918. It was a prestigious appointment at a major institution committed to developing its capacity for advanced research. He appears to have been a popular and highly competent professor and administrator during a period when the faculty of medicine and his department were experiencing considerable growth and modernization, spiced by controversial issues ranging from terms of appointment to the treatment of laboratory animals. He had at his disposal exceptionally good research facilities and support and was satisfied enough with his position to refuse a request to become a candidate for the widely esteemed chair of physiology at Johns Hopkins Hospital and School of Medicine.
On November 8, 1920, Macleod was asked by Frederick Grant Banting*, a medical graduate of the University of Toronto, if he could make facilities available for Banting to test an idea he had developed to try to isolate the long-sought internal secretion of the pancreas, a substance which, if it existed, appeared to be necessary for normal metabolism, particularly the avoidance of diabetes mellitus. Macleod told the young doctor, who knew little about research and less about diabetes, that he would probably achieve negative results with the idea, but he agreed that even these would make it worth trying. If the work accomplished nothing else, Macleod knew he had a mandate from the university to develop its research capacity. When Banting came back to Toronto in May 1921, Macleod assigned him laboratory space, a supply of dogs to use in his experiments, and the services of his student assistants over the summer. He instructed Banting on surgical procedures and the plan of research before leaving for Scotland in mid-June.
When Banting and his assistant, Charles Herbert Best*, reported positive results to Macleod later that summer and on his return to Toronto in September, he advised them to repeat and refine their experiments to build a convincing case that the elusive secretion was being located. As head of the lab, he rejected Banting’s demands for priority for his project, but he gradually became increasingly interested in what seemed to be a pattern of favourable results. In December he acceded to Banting’s request to add an experienced biochemist, James Bertram Collip*, to the team, and he sponsored a report on Banting and Best’s experiments to the American Physiological Society on 30 December. As formal director of the research project, Macleod arranged the clinical trials on human subjects that began in January 1922 and showed spectacular success after Collip succeeded in purifying Banting and Best’s extracts (first of dog and then of beef and pork pancreas), which had often, though not always, been successful on dogs. A fast-moving, exciting scientific adventure suddenly became enmeshed in personal antagonisms when Banting began accusing Macleod and Collip of appropriating credit for his discovery. As he steered the investigation towards triumphant publication later that spring, Macleod had to arbitrate violent conflict between Banting and Collip, while also defending himself against Banting’s charges of unethical behaviour.
In 1922-23 Macleod organized ongoing research into the characteristics of the substance he suggested be called insulin (after the islet cells in the pancreas where the group assumed it was produced; he subsequently realized that earlier researchers had suggested a similar name for the hypothetical secretion), packaged and presented the discovery to the scientific world, and negotiated a delicate course through early production problems and clinical trials. He maintained his equanimity through a series of further misunderstandings with Banting. While Banting and his friends were able to convince Canadian authorities that there was only one principal discoverer of insulin (with some help from Best), other scientists and the Nobel Committee for Physiology or Medicine in Sweden concluded that Banting could not have reached insulin without Macleod’s guidance and recommended that the 1923 prize be awarded jointly to Banting and Macleod. Banting divided his prize money equally with Best; Macleod split his with Collip.
Macleod continued to supervise important ongoing research into the physiology of insulin at Toronto but found the atmosphere poisoned by Banting’s continuing rancour. Perhaps also eager to return to his native land, he left Canada in 1928 to become regius professor of physiology at the University of Aberdeen. Fully honoured in Scotland, Macleod made further useful research contributions; his return to an earlier interest in the possibility of neurogenesis of diabetes led some of his students, such as Hans Kosterlitz, to become pioneers in work on endorphins many years later. In semi-retirement Macleod was a gentle, quiet man and a lover of music and art, especially Canadian painting (in Toronto he had briefly been a member of the city’s Arts and Letters Club). He died from the effects of arthritis in 1935.
The persistence in popular and even some scientific circles of the view that Macleod had stolen credit from Banting and Best continued to cloud his reputation. Serious historical reconsideration began after the death of Best in 1978 and the ensuing publication of Macleod’s 1922 account of the events in Toronto. It is now recognized that Macleod, along with Collip, played an essential role in the discovery of insulin. The event emerges as an early example of a breakthrough achieved by scientific collaboration – fractiousness notwithstanding – in a well-equipped research university. An expert, cautious, patient, and wise scientist, J. J. R. Macleod gradually became recognized even in Canada and at the University of Toronto for his leadership in the finest research achievement in the country during the 20th century.
In addition to the titles mentioned in the biography, J. J. R. Macleod is the author or co-author of 9 monographs and some 200 scientific papers. Details about much of his published work appear in M. J. Williams, J. J. R. Macleod: the co-discoverer of insulin (Edinburgh, 1993), a slightly hagiographic but generally thorough and authoritative biography. Numerous of his publications during and after the insulin research in Toronto contain brief, carefully phrased accounts of the work, most notably, J. J. R. Macleod and W. R. Campbell, Insulin: its use in the treatment of diabetes (Baltimore, Md, 1925). His long-suppressed, 5,000-word memoir of his role in the discovery, written in September 1922 at the invitation of Albert Edward Gooderham, chairman of the Univ. of Toronto’s insulin committee, was published as “History of the researches leading to the discovery of insulin,” intro. L. G. Stevenson, Bull. of the Hist. of Medicine (Baltimore), 52 (1978): 295-312. It may be compared with “Banting’s, Best’s, and Collip’s accounts of the discovery of insulin,” intro. Michael Bliss, Bull. of the Hist. of Medicine, 56 (1982): 554-68.
Extensive enquiries in Scotland and Canada have failed to uncover a major collection of Macleod papers. A substantial amount of his correspondence during the insulin years survives in the Charles Herbert Best papers (ms coll. 241) in the Thomas Fisher Rare Book Library, Univ. of Toronto. A number of the letters, along with details of the Fisher Library’s other extensive insulin collections, notably the Sir Frederick Grant Banting papers (ms coll. 76), are available online at the Univ. of Toronto Libraries, Fisher Library Digital Coll., “The discovery and early development of insulin”: link.library.utoronto.ca/insulin (consulted 5 Nov. 2014).
The standard published history of the research, which draws on all the primary sources, is Michael Bliss, The Discovery of Insulin (Toronto, 1982; 25th anniversary ed., 2007). Special attention to Macleod’s scientific career before and after insulin is given in Michael Bliss, “J. J. R. Macleod and the discovery of insulin,” Quarterly Journal of Experimental Physiology (Cambridge, Mass.), 74 (1989): 87-96. The discovery is set in the context of the history of the Univ. of Toronto and its medical faculty in M. L. Friedland, The University of Toronto: a history (Toronto, 2002).
NRS, SR Births, Caputh (Perth), 6 Sept. 1876; SR Deaths, Peterculter East (Aberdeen), 16 March 1935; SR Marriages, Paisley (Renfrew), 22 July 1903.
James Collip
James Bertram Collip, a biochemist, endocrinologist, university teacher, medical-research administrator, and office holder was born November 20, 1892, in Belleville, Ontario. Elder of the two children and only son of James Dennis Collip, a gardener and florist, and Mahala Frances Vance, a schoolteacher; m. 28 Dec. 1915 Ray Vivian Margaret Ralph in Dundas, Ont., and they had two daughters and a son; d. 19 June 1965 in London, Ontario.
James Bertram Collip, known to his family and friends as Bert attended a one-room country school and Belleville High School, where he developed an interest in science, particularly chemistry. In 1908 he entered Trinity College, which had recently federated with the University of Toronto. Because, at the age of 15, he was too young to pursue the medical course as he had intended, he enrolled in Honours Physiology and Biochemistry, a program that provided rigorous training in original research for an elite stream of medical students. Collip received a BA in 1912 and graduated at the head of his class. He then undertook studies in biochemistry with Archibald Byron Macallum* and earned an MA in 1913 and a PhD three years later for his research on the formation of hydrochloric acid in the vertebrate stomach. During his student days, he met Ray Ralph, who was an art student at Trinity College; they married in 1915.
That year Collip was appointed a lecturer in biochemistry in the Department of Physiology at the University of Alberta, where he would carry on an active research program on the blood chemistry of vertebrates and invertebrates. After the close of World War I, he was awarded a Rockefeller Travelling Fellowship that allowed him to go elsewhere during his sabbatical year in 1921-22. In April 1921 he returned to the University of Toronto on the first stop of his intended journey, which was also to take him to New York and England, and began studies with John James Rickard Macleod*, a renowned authority on carbohydrate metabolism. After a summer spent visiting marine biological stations at Woods Hole, Mass., and St Andrews, N.B., Collip, with his wife and young family, settled in Toronto for the autumn.
In December he was asked to contribute his skills as a biochemist to a promising research project that was being carried out under Macleod’s supervision. Frederick Grant Banting*, a physician from London, Ont., and Charles Herbert Best*, a student in the honours physiology and biochemistry program, were searching for the active principle of the pancreas, which Banting believed could be used to treat diabetes mellitus. Over the summer and autumn of 1921, they had successfully made an extract, first from dogs and later from cattle, that could lower blood sugar. However, this preparation proved to be unsuitable for clinical use because its impurities caused undesirable side effects, especially the formation of a sterile abscess at the site of the subcutaneous injection. Banting and Best had an anti-diabetic agent in their extract, but they had achieved no more than other researchers before them, notably Georg Ludwig Zuelzer (1908), Ernest Lyman Scott (1912), Israel S. Kleiner (1919), and Nicolas Constantin Paulescu (1921).
Recognizing the need for a more purified product, Banting asked Macleod to invite Collip to join in the work. On 19 Jan. 1922 Collip prepared an extract by using increasing concentrations of alcohol. He found that impurities were thrown down at up to 80 percent ethyl alcohol and that the active principle precipitated out in pure form at around 95 percent alcohol. This extract was the first one suitable for clinical use, as was demonstrated in a successful trial on diabetic patient Leonard Thompson on 23 January.
Collip also made key physiological observations. First, he described acute hypoglycemia in normal rabbits that were given a dose of the extract; the animals suffered convulsions and then became comatose. He demonstrated that this effect was the result of dangerously low blood sugar and that it could be corrected by the injection of a glucose solution. Because of this finding, Collip was able to warn clinicians of the dangers of hypoglycemia following too-high doses of the extract. As well, he developed a biological assay for the preparation by measuring its effect on the blood sugar of normal rabbits, which meant the extract could be standardized more easily and economically than by using depancreatized dogs. Secondly, he showed that glucose in the blood was converted to glycogen in the liver following the administration of the extract. This outcome was proof that the extract replaced a physiological function that was missing in the diabetic patient. Finally, Collip demonstrated that ketones in the blood and urine were eliminated when the extract was used.
These pieces of evidence were crucial because Banting and Best had demonstrated only the extract’s effect in reducing glucose in blood and urine; however, lowered sugar output might be the result of other conditions, such as a reaction to toxic elements in the extract, rather than replacement of the actual function of the pancreas. In providing a non-toxic anti-diabetic extract suitable for therapeutic use and in describing key physiological properties of the active principle’s action, Collip extended the work of the Toronto group beyond what had been accomplished by other researchers and provided convincing proof of the product’s value in treating diabetes. Unfortunately, relations among the discoverers became fraught, as Banting grew anxious that Macleod and Collip were taking credit away from him. An angry confrontation broke out when Collip announced that he had purified the extract but refused to divulge his method, having been advised by Macleod and others to keep it secret until it had been fully tested.
Initially, quantities of the product were frustratingly small, even as demand for it grew when news of the team’s success spread. The researchers worked with the University of Toronto’s Connaught Antitoxin Laboratories, under John Gerald FitzGerald*, to increase the production of the extract, which was given the name insulin. Later it became clear that more resources were needed, and the pharmaceutical firm Eli Lilly and Company of Indianapolis, Ind., collaborated with the Toronto group to manufacture insulin on a commercial scale. A patent was taken out in 1922 in the names of Banting, Best, and Collip and turned over to the University of Toronto’s Board of Governors to manage. Royalties were split: half was directed to the university for a research fund and the rest was divided among the three researchers for the support of their work wherever they went in Canada. This arrangement, together with grants from several organizations, meant that Collip had access to what would be the largest ongoing funding for medical research available in the country at the time.
Banting and Macleod were awarded the Nobel Prize in Physiology or Medicine in 1923. Banting announced that he would share his award money with Best, and Macleod followed suit by stating that he would share his with Collip in recognition of the young researcher’s role in the discovery. Collip had given up his Rockefeller fellowship in early 1922 to remain at the University of Toronto until the end of his leave. When he returned to the University of Alberta later that year, as a full professor and head of the department of biochemistry, he moved away from general research in that field and would thenceforth focus exclusively on the identification and isolation of hormones of therapeutic value. To further his work in this new area, he enrolled in medical school as a part-time student and earned an MD in 1926, while continuing to serve as a faculty member. He had been awarded a dsc two years earlier for his research accomplishments.
A skilled laboratory biochemist, Collip was a leading researcher in endocrine science during the 1920s and 1930s. His most important contribution in the first years after the insulin discovery was the isolation in 1924 of the parathyroid hormone, which could be used to treat parathyroid tetany. Collip and chemist Earl Perry Clark provided evidence that this hormone regulates serum calcium and that low levels of calcium in the blood result in tetany. They also developed a method for measuring serum calcium that would be standard in laboratories for decades. However, as a result of his research, Collip found himself embroiled in a dispute over priority with Minnesota physician Adolph Melanchthon Hanson, who in 1923 had published a method of preparing an extract of the parathyroid gland using hot hydrochloric acid, a year earlier than Collip’s paper describing the same procedure. In 1932 Hanson was awarded the American patent for the product and process of extracting the principle of the parathyroid gland. Yet Collip is generally recognized by the scientific community for isolating the hormone, providing physiological proof of its activity, and contributing to the growth of the scientific study of the parathyroid.
In 1928 Collip, having turned down an offer from the prestigious Mayo Clinic in the United States, was appointed to the chair of biochemistry at McGill University, succeeding his mentor A. B. Macallum. There he headed a large, thriving research team that included David Landsborough Thomson, Hans Hugo Bruno Selye*, and graduate students John Symonds Lyon Browne, Evelyn M. Anderson, and Leonard Irving Pugsley*. Throughout his career, he was ably assisted by his loyal factotum, Arthur Long, who had joined his laboratory at the University of Alberta after the war and followed him to McGill and, later, to the University of Western Ontario.
The field of endocrinology was burgeoning in the 1930s, and there was tremendous scientific interest in sex hormones and in the pituitary gland, which was understood to be the master gland controlling the function of several others. An interdisciplinary approach was necessary. Collip, the biochemist, provided the extracts by distilling the active principles from the raw materials. Selye, the histologist, was skilled in surgical techniques and mastered the difficult preparation of the rats to be used as test animals by removing their pituitaries via a parapharyngeal route. He also supplied the histological studies that were required when the hormones associated with growth and development were studied. The biochemical and physiological functions of Collip’s extracts were explored by other members of the team. The McGill group and several laboratories around the world were actively involved in extracting various components of the anterior pituitary gland and describing their functions; they identified hormones that stimulated the thyroid, the adrenal cortex, and growth. Collip, Anderson, and Thomson prepared a crude but active extract of adrenocorticotropic hormone (ACTH) in 1933 that was sufficiently pure for clinical use.
Collip was entrepreneurial in expanding and sustaining his research ventures by negotiating with administrators, finding private donors, and forging alliances with business enterprises. In 1930 he isolated what he called Emmenin, a form of estriol from the placenta that was commercially significant because it could be administered by mouth. He collaborated with the small Montreal pharmaceutical firm Ayerst, McKenna and Harrison, which expanded its research and manufacturing operations to advance this product. Later the Ayerst researchers would develop a different orally active estrogen from pregnant mares’ urine called Premarin. Used in hormone replacement therapy for the treatment of menopausal symptoms, it became one of the top-selling pharmaceutical products in the second half of the 20th century and established Ayerst as a major player in the field. The company advertised that Emmenin and Premarin had been standardized in Collip’s laboratory and paid royalties on both products, providing the lab with considerable research funds for decades, which were particularly important at a time when government support had not yet begun and when researchers were dependent on private donors and foundations.
Collip was known for his restless nature and for the speed with which he thought, spoke, and made decisions. Students and associates fondly remember his habit of driving very fast, and a car trip with him was, a colleague remarked, akin to “a form of low flying.” During the McGill years, Collip spent long hours at his large distillation units, making extracts from huge numbers of glands provided by the slaughterhouse and placentas supplied by the maternity hospitals. He rushed back and forth adjusting this or that mixture, smoking large hand-rolled cigarettes, and dropping ashes on his vest. Many students and postdoctoral fellows passed through the lab and thrived in an atmosphere of enthusiasm and productivity. Collip relished this environment and was full of ideas when something captured his interest, but he let his co-workers and students pursue their projects. He had a lifelong habit of working late into the night, and his wife, Ray, often came in to keep him company. A gracious and supportive partner throughout their marriage who was familiar with her husband’s penchant for quick changes in plans, she learned to keep a suitcase packed and ready. In later years his younger daughter, Barbara Vivian, joined him in the lab and sometimes found herself sitting with a dropper and instructions not to let something boil over.
Between 1938 and 1957 Collip took a leading role in establishing federal coordination and funding of medical research through the National Research Council of Canada (NRC). In the mid-1930s he had become reconciled with Banting, and when Banting organized the Associate Committee on Medical Research for the NRC in 1938, he asked Collip to join. Collip was the last friend and colleague to see Banting before he died following a plane crash in 1941. After his death, Collip assumed leadership of the medical research arms of the NRC, including the heavy wartime responsibility of overseeing associate committees for each of the three branches of the armed forces and serving as Canada’s medical liaison officer to Washington. He was an acting lieutenant colonel in the Royal Canadian Army Medical Corps from 1942 and acting colonel from 1944. When the Division of Medical Research replaced the Associate Committee on Medical Research in 1946, he was appointed its first director, and he helped to shape government support for work across the country. Because of Canada’s small population, Collip argued against building national laboratories like those in Britain and the United States; instead, he promoted grants-in-aid for research at universities and teaching hospitals.
A Gilman Cheney chair in endocrinology had been created for Collip at McGill in 1937, and four years later, at his urging, the university established the Research Institute of Endocrinology. But in 1947 he accepted an invitation to become dean of medicine at the University of Western Ontario in London. He enjoyed the challenge of building up its medical school during an era of active expansion. He was also a professor and head of the Department of Medical Research, though he was no longer actively involved in such work. At the Collip Medical Research Laboratory in 1958 his long-time associate Robert Laing Noble, who had followed him to Western, and biochemist Charles Thomas Beer isolated vinblastine, a drug that became one of the key elements in combination chemotherapy for cancer.
Collip received many honours during his career. He was made a commander of the Order of the British Empire in 1943 and awarded the American Medal of Freedom with Silver Palm four years later for his war efforts. He had been elected a fellow of the Royal Society of Canada in 1925 and served as its president in 1942-43. He was also a fellow of the Royal Society of London from 1933. He went on to win the Flavelle Medal of the Royal Society of Canada and the F. N. G. Starr Award of the Canadian Medical Association in 1936, the Cameron Prize from the University of Edinburgh in 1937, the Charles Mickle Fellowship Award from the University of Toronto in 1941, and the Banting Medal for Scientific Achievement of the American Diabetes Association in 1960. Twelve honorary degrees were conferred on him by universities in Canada, Britain, and the United States. Collip retired from the NRC in 1957 and as dean of medicine four years later. He remained head of the Collip Medical Research Laboratory and continued to be interested in its activities, but he never went back to the bench himself. He died of a stroke at the age of 72, two days after returning home from a cross-country trip with Ray to attend the annual meeting of the Royal Society of Canada in Vancouver.
Skilled both as a laboratory scientist and as an entrepreneur, James Bertram Collip was a pioneering researcher in endocrinology and a leader in the development of Canadian medical research. He was at the forefront of the institutional transformation of medical science, which, in the opening decades of the 20th century, had been the pursuit of a select few but which, by mid-century, had grown into a large-scale, systematic venture that involved teams of professional scientists and dozens of laboratories in universities, government, and industry. Collip’s role in insulin discovery was recognized by only a small circle and largely forgotten by the general public, who credited Banting and Best with the achievement. In recent decades, however, the critical importance of his work to the success of the Toronto group has become more widely acknowledged. He found the bitter conflict associated with the discovery distasteful. Known for his integrity, modesty, and quiet nature, Bert Collip always refused to discuss the insulin days, saying only that he was sure the historical record would speak for itself.
James Bertram Collip has a full-length biography in Alison Li, J. B. Collip and the development of medical research in Canada: extracts and enterprise (Montreal and Kingston, Ont., 2003). M. L. Barr and R. J. Rossiter, “James Bertram Collip, 1892-1965,” Royal Soc. of London, Biog. memoirs of fellows, 19 (1973): 235-67, an excellent account of his life, also contains a bibliography of Collip’s published work. Short biographical sketches and reminiscences of the scientist can be found in J. S. L. Browne and O. F. Denstedt, “James Bertram Collip (1892-1965),” Endocrinology (Philadelphia), 79 (1966): 225-28; D. A. Keys, “James Bertram Collip …: an appreciation,” Canadian Medical Assoc., Journal (Toronto), 93 (1965): 774-75; R. L. Noble, “Memories of James Bertram Collip,” Canadian Medical Assoc., Journal, 93 (1965): 1356-64; and R. J. Rossiter, “James Bertram Collip, 1892-1965,” Royal Soc. of Can., Trans. (Ottawa), 4th ser., 4 (1966), proc.: 73-82.
Michael Bliss reveals crucial details of Collip’s role in the events of 1921-22 in The Discovery of Insulin (Toronto, 1982; 25th anniversary ed., 2007), and he evaluates the scientist’s legacy in “J. B. Collip: a forgotten member of the insulin team,” in Essays in the history of Canadian medicine, ed. Wendy Mitchinson and Janice Dickin McGinnis (Toronto, 1988), 110-25, and “Rewriting medical history: Charles Best and the Banting and Best myth,” Journal of the Hist. of Medicine and Allied Sciences (New Haven, Conn.), 48 (1993): 253-74. Collip’s itemized list of his contributions to insulin research was published in “Banting’s, Best’s, and Collip’s accounts of the discovery of insulin,” intro. Michael Bliss, Bull. of the Hist. of Medicine (Baltimore, Md), 56 (1982): 554-68.
Collip’s research on the physiology of the parathyroid hormone is examined in T. B. Schwartz, “Giants with tunnel vision: the Albright-Collip controversy,” Perspectives in Biology and Medicine (Chicago), 34 (1991): 327-46, which focuses particularly on his disagreement with American endocrinologist Fuller Albright. Virginie Marier and Tina Piper describe the scientist as an innovator in the development of business models for the commercialization of medical science and the protection of intellectual property in “Early twentieth-century Canadian medical patent law in practice: James Bertram Collip and the discovery of Emmenin,” Univ. of Toronto Law Journal, 60 (2010): 855-91.
Arch. of Ont. (Toronto), RG 80-2-0-379, no.12682; RG 80-5-0-812, no.16756. McGill Univ. Arch. (Montreal), RG 38 (Faculty of Medicine). Univ. of Alta Arch. (Edmonton), Henry Marshall Tory fonds. Univ. of Toronto Libraries, Thomas Fisher Rare Book Library, ms coll. 269 (James Bertram Collip papers). Western Univ. Arch. (London, Ont.), James Bertram Collip fonds.